Our immune system is primarily viewed as a safeguard mechanism that limits pathogenic infiltration. But what if there is chaos inside one’s own system? The system needs to be restrained and ‘tolerized’ from fighting against its own self and stopped from compromising its own health. Such a job of paramount importance is performed by a specialized type of white blood cells called Regulatory T cells (Treg cells). When self-destructive immune cells are in the verge of triggering autoimmunity and the body is in a chaotic state of war acting on misleading signals and commands leading to more destruction, the Treg cells act as peace keeping force by applying a much needed brake on the hyper-immune reactions in the body.Treg cells are thereby absolutely essential to restrain excessive inflammatory responses leading to fatal autoimmune diseases.
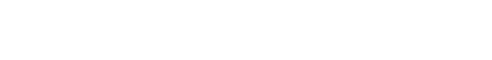
Contrary to their healing role in the context of autoimmune diseases, Treg cells have a darker side when it comes to cancer. Within tumors, where the immune system continuously battles against excessive growth and proliferation of tumor cells, Treg cells are obstructive, as they counteract the function of other immune cells, resulting in happy growth of tumors. Due to such two-pronged functions, Treg cells are pursued extensively as a promising therapeutic supplement in the context of autoimmunity as well as targets in the context of cancer. It is therefore of utmost importance to understand how Treg cells become what they are and acquire such immune-regulatory functions in the first place.
Just like our parental genes determine who we are, the Treg cells have a transcription factor called Foxp3 that defines them. Foxp3 is exquisitely expressed in Treg cells and its loss leads to catastrophic autoimmunity in humans as well as in mice, which are model organisms where most of the experiments are performed in order to determine Treg cell functionality. Foxp3, by working together with numerous other factors, and by binding to specific regions of DNA, determine which genes need to be switched on or off in Treg cells to make them what they are. It therefore serves as a “master” regulator that shapes up the “genetic signature” of Treg cells that is required for their seamless function and overall organismal health.
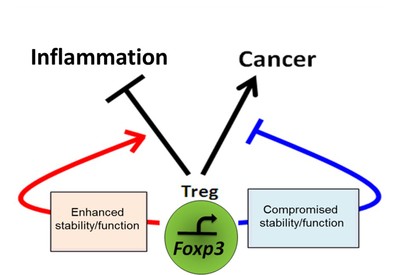
Although identified in the context of dominant tolerance of the immune system, with time it is becoming increasingly clear that apart from being instrumental in suppressing inflammatory responses, Treg cells have evolved to execute several non-immune functions related to tissue homeostasis, and thereby assimilate into a larger biological paradigm for overall organismal health. For example, current research implies a role of Treg cells in various non-immune functions like tissue healing and regeneraton, protection against brain damage, and believe it or not, to maintain a proper hair follicle cycle, an alteration of which would lead to inappropriate hair loss. For more comprehensive understanding of the multifaceted functions of Treg cells and their therapeutic potentials in clinical setting, please go through the following two review articles we wrote:
https://www.frontiersin.org/articles/10.3389/fimmu.2018.00883/full
https://www.tandfonline.com/doi/abs/10.1080/08830185.2019.1621310?journalCode=iiri20
Research in our laboratory is focused on dissecting the cellular, molecular and metabolic features that are responsible for governing Treg functions in controlling systemic inflammation, exerting its 'non-immune' functions in maintaining tissue homeostasis, as well as in regulating anti-tumor immunity, with the long-term goal of employing this knowledge in utilizing and targeting Treg cells in clinical settings of autoimmunity, metabolic inflammation and cancer.